Electrophysiology Studies
Electrophysiology studies (EP studies) are tests that help health care professionals understand the cause of abnormal heart rhythms (arrhythmias).
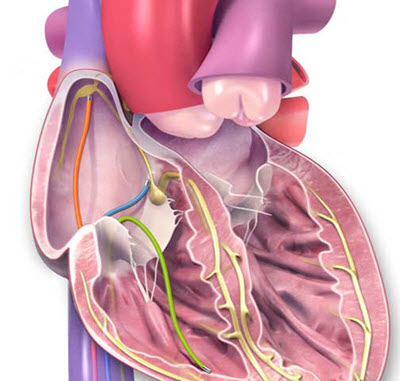
Electrophysiologic testing uses catheters inserted into the heart to find out where abnormal heartbeats are coming from.
During an EP study, a thin tube called a catheter is inserted into a blood vessel that leads to your heart. Specialized electrodes are then placed in the heart to send electrical signals and measure electrical activity in your heart.
EP studies are used to see:
- Where an arrhythmia is coming from
- How well certain medications work to treat your arrhythmia
- Whether to treat a problem by destroying the place inside your heart that is causing the abnormal electrical signal. This procedure is called catheter ablation
- If a pacemaker or implantable cardioverter defibrillator (ICD) might help you
- If you are at risk for heart problems such as fainting or sudden cardiac death due to cardiac arrest
What are the risks of EP studies?
In most cases, the procedure is very safe. Discuss this with your health care professional. Some possible risks may include:
- Arrhythmia. During an EP study, you may have abnormal heart rhythms that make you dizzy. If this happens, your health care professional may give your heart an electric shock to bring back a regular heartbeat.
- Heart attack (myocardial infarction) and stroke
- Heart valve damage
- Blood clots sometimes can form at the tip of the catheter, break off and block a blood vessel. Your health care professional may give you medicine to prevent blood clots.
- Infection, bleeding and bruising at the site where the catheter went in (groin, arm or neck). Your doctor or nurse will help you avoid these problems.
How do I prepare for the test?
- Don’t eat or drink for six to eight hours before the test.
- Tell your health care professional about any medications you take, including over-the-counter medications, herbs and vitamins. They may ask you not to take them before the test. Don’t stop taking your medication until your health care professional tells you to.
- Have someone drive you to your appointment and take you home.
- If you usually wear a hearing aid, wear it during your procedure. If you wear glasses, bring them to your appointment.
What happens during the EP study?
At a hospital or clinic, doctors and nurses do an EP study in a room that has special equipment for the tests. You may hear this room called the electrophysiology laboratory, or EP lab. Some call it the catheterization laboratory (cath lab). During the test:
- A nurse will put an IV in your arm. You’ll get medication (a sedative) that will help you relax. But you’ll be awake and able to follow instructions during the test.
- Your nurse will clean and shave the part of your body where the doctor will be working. This is usually in the groin but may be the arm or neck.
- You’ll be given a shot (a local anesthetic) to make the area numb. Your doctor will make a needle puncture through your skin and into your blood vessel. A small straw-sized tube called a sheath will be inserted into your artery or vein. Then several specialized EP catheters will be guided into your blood vessel through the sheath and advanced to your heart. A video screen will show the position of the catheters. You may feel some pressure in the area where the sheath was inserted, but you shouldn’t feel any pain.
- Your doctor will send small electric pulses through the catheters to make your heart beat at different speeds. You may feel your heart beat stronger or faster.
- Electrical signals produced by your heart will be picked up by the special catheters and recorded. This is called cardiac mapping and allows the doctor to locate where arrhythmias are coming from.
- Your doctor will remove the catheters and the IV line. Your nurse will put pressure on the puncture site to stop any bleeding.
- The test usually lasts one to four hours.
If the type and location of the abnormal heart rhythm is identified and an appropriate therapy decided, cardiac ablation or insertion of a pacemaker or ICD may be performed during or right after the EP study.
What happens after the test?
You’ll be moved to a recovery room for one to three hours. During this time:
- Stay still as long as your nurse tells you to. Be sure to keep the arm or leg used for the test straight.
- Your nurse will check for bleeding or swelling at the puncture site.
- Before you leave, you’ll be told what to do at home.
What happens after I get home?
Follow the instructions your health care professional gave you, including taking any new medications that were prescribed. Most people can start eating food and taking their medications within four to six hours after the test. Most can do their usual daily activities the day after the test. Don’t drive for at least 24 hours.
The puncture site may be sore for several days. A small bruise at the puncture site is normal. If the site starts to bleed, lie flat and press firmly on top of it. Have someone call your health care professional or the EP lab.
What should I watch for?
Call 911 if you notice:
- Any symptoms of pain or tightness in the chest or signs of stroke (face drooping, arm weakness, speech difficulties)
- A sudden increase in swelling around the puncture site
- Bleeding that doesn’t slow down when you press hard on the site
Call your health care professional right away if you notice:
- Your arm or leg used for the catheter feeling numb or tingling
- Your affected hand or foot feeling very cold or changing color
- The puncture site looking more and more bruised
- The puncture site beginning to swell or fluids coming from it
- Fever
- Shortness of breath
When will I know the results of my EP study?
Most of the time, your health care professional will ask you to make an appointment to discuss your test results. You’ll discuss your treatment options at that appointment.
Access a printable sheet: What are Electrophysiology Studies? (PDF)