Recurrent Pericarditis

What is recurrent pericarditis?
Recurrent pericarditis is when you develop pericarditis for a second time after having no symptoms for at least four weeks.
Pericarditis is inflammation of the pericardium, a sac-like organ with two thin layers of tissue that surround the heart. The pericardium holds the heart in place, protects it from infection, and keeps it from filling with too much blood. It also cushions the heart from outside pressure. A small amount of fluid keeps the layers separate and decreases the friction between them as the heart beats. But in some people with this condition, these tissues become swollen and irritated. This can cause sharp chest pain and may lead to fluid buildup around the heart that causes discomfort. In most cases, pericarditis is mild and gets better on its own without treatment.
Among those treated for acute pericarditis, 15% to 30%, or nearly 40,000 people in the United States, may experience recurrent pericarditis if not treated with the medication colchicine. Pericarditis is most common in men 16 to 65 years old, but it can affect anybody at any age. About 5% of people seeking treatment in emergency departments for chest pain had acute pericarditis.
Other types of pericarditis include:
- Acute pericarditis lasts less than four to six weeks.
- Incessant pericarditis symptoms last more than four to six weeks but less than three months despite therapy.
- Chronic pericarditis lasts for more than three months.
View sheet: Recurrent Pericarditis (PDF)
What are the symptoms of recurrent pericarditis?
Symptoms of recurrent pericarditis include:
- Chest pain is almost always present. It may feel like a sharp, stabbing pain that radiates to the arm, neck, shoulder, back or abdomen. Some people mistake the pain for a heart attack. The pain gets worse when coughing, taking deep breaths or lying down. The pain may improve by sitting up and leaning forward.
- Shortness of breath or difficulty breathing
- Heart palpitations or a faster than normal heartbeat
- Low-grade fever, chills or sweating
- Dry cough
- Swollen abdomen, legs or feet
- Low blood pressure symptoms, such as lightheadedness, dizziness or fainting
What causes recurrent pericarditis?
The cause of recurrent pericarditis is idiopathic, or unknown, in most patients. While there’s no single cause for recurrent pericarditis, it often develops in people whose initial bout of pericarditis isn’t treated adequately.
Viral illnesses, such as herpes, influenza, adenovirus, enterovirus or Epstein Barr virus may also cause recurrent pericarditis.
Other potential causes include:
- Autoimmune conditions such as lupus, scleroderma and rheumatoid arthritis
- Complications from a heart attack or heart surgery
- Health problems, such as kidney failure or cancer
- Bacterial, fungal and parasitic infections (most common in people with compromised immune systems)
- Radiation to the chest
- Chest trauma
- Certain medications, such as phenytoin (an anti-seizure medicine) and procainamide (prescribed for irregular heartbeats)
How is recurrent pericarditis diagnosed?
Depending on your age and medical conditions, a primary care doctor, cardiologist, rheumatologist or infectious disease specialist may treat you.
If your doctor believes you may have pericarditis, they’ll listen to your heart for rubbing sounds that often occur in people with the condition. One or more of the following tests may be used to confirm the diagnosis:
- Blood test: May reveal elevations in the white blood cell count, erythrocyte sedimentation rate, and serum C-reactive protein concentration and other signs of inflammation.
- EKG (electrocardiogram): Measures your heart’s electrical activity and certain results may suggest pericarditis.
- Chest X-ray: Takes pictures of the heart, lungs and blood vessels inside your chest. An X-ray can show whether the heart is enlarged due to excess fluid in the pericardium. It may also reveal signs of infection, sarcoidosis or malignancies that may cause pericarditis.
- Echocardiogram: Sound waves create pictures of your heart’s size, shape and how it’s working. This can reveal fluid buildup in the pericardium.
- Cardiac CT (computed tomography): A type of X-ray that takes a clear, detailed picture of your heart.
- Cardiac MRI (magnetic resonance imaging): Also called CMR, this test uses magnets and radio waves to create detailed images of your organs and tissues. This can reveal changes in the pericardium.
How is recurrent pericarditis treated?
Recurrent pericarditis is usually treated with the anti-inflammatory drug colchicine and aspirin and non-steroidal anti-inflammatory drugs (NSAIDS).
When NSAIDs and colchicine don’t lead to a complete resolution, low to moderate doses of corticosteroids, such as prednisone may also be prescribed. Because steroids have been linked with a higher risk of recurrence, they’re typically used in people who can’t tolerate NSAIDs or colchicine or in those who are pregnant or have conditions such as autoimmune disease.
Immunosuppressants, anti-inflammatory and interleukin 1 blockers, which neutralize pro-inflammatory molecules, may also be prescribed for patients who don’t respond to medications to achieve better symptom control.
Your doctor may perform a pericardiocentesis where excess fluid is drained from the pericardium. Or as a last result, the pericardium may be removed partially or entirely. This is called a pericardiectomy.
Outlook
For most people, recurrent pericarditis can be safely managed at home and rarely leads to death. But it can cause potentially life-threatening complications, such as loss of the pericardium’s elasticity (constrictive pericarditis) and a buildup of fluid in the pericardium (cardiac tamponade). Some people with pericarditis may also have pericardial thickening.
Seek medical treatment if you have continued symptoms of pericarditis.
If you feel chest pain of any type, immediately call 911 because it may be a sign of a heart attack. If you have recurrent pericarditis, be sure to talk to your doctor about your symptoms and treatment options.
View an Answers by Heart sheet: What Is Recurrent Pericarditis? (PDF)
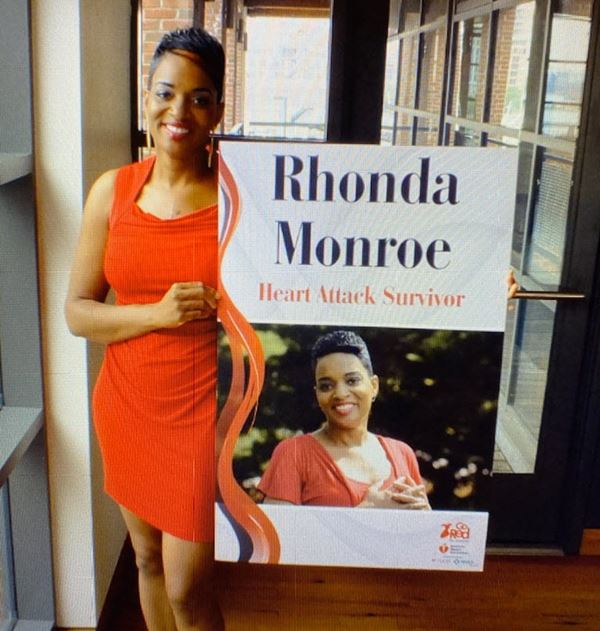
I Survived and Thrived After a Yearlong Bout with Recurrent Pericarditis