Tachycardia: Fast Heart Rate
The normal rate for a heart to beat is 60-100 beats per minute. Tachycardia is when the heart beats too fast, at a rate of more than 100 beats per minute, when at rest. This can depend on age, health status and physical condition. Learn about the types of tachycardias:
- Supraventricular Tachycardia (SVT)/ Paroxysmal Supraventricular Tachycardia (PSVT)
- Sinus Tachycardia
- Ventricular Tachycardia

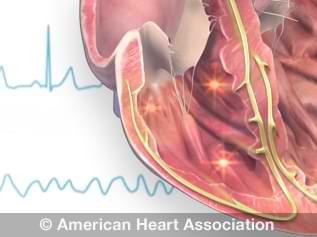
ECG strip showing a normal heartbeat

Supraventricular Tachycardia (SVT)/ Paroxysmal Supraventricular Tachycardia (PSVT)
SVT is also known as atrial tachycardia. It is a fast heart rate, greater than 100 beats per minute or more, which starts in the atria, the upper chambers of the heart. The electrical signals occur abnormally and speed up the heart rate. The rapidly beating heart prevents the heart chambers from filling completely between contractions (beats), which may compromise blood flow to the body.
SVT is the most common heart arrhythmia in infants and children. Paroxysmal SVT means that the abnormality may come and go over minutes or days.
View an animation of tachycardia.
Risk factors for SVT/PSVT
- Anxiety and stress
- People middle age and older
- Women more than men
- Children (SVT is the most common heart arrhythmia in children)
For some people, SVT/PSVT is triggered by exercise, stress or lack of sleep, while others do not notice anything at all.
Issues that may cause an SVT episode include:
- Age
- Anemia
- Heart disease
- Dehydration
- Coronary artery disease; having had cardiac surgery or other heart problems
- Congenital heart disease
- Other heart conditions, such as Wolff-Parkinson-White syndrome
- Chronic lung disease
- Excessive caffeine intake
- Excessive alcohol intake
- Smoking or other tobacco products, drug misuse, including cocaine and methamphetamines.
- Pregnancy
- Menopause
- High blood pressure
- Certain over-the-counter medications, including those for asthma, colds and allergies.
Symptoms of SVT/PSVT
- Very fast (rapid) heartbeat that may come and go
- A fluttering or pounding in the chest (palpitations)
- A bounding pulse sensation in the neck
- Weakness or feeling very tired (fatigue)
- Chest discomfort
- Shortness of breath
- Lightheadedness or dizziness
- Sweating
- Fainting (syncope) or near fainting
- Nausea
How SVT/PSVT is diagnosed
SVT
After giving a detailed medical history (including asking about potential causes) and a list of symptoms to a health care professional, patients will be advised to get an electrocardiogram (ECG or EKG).
PSVT
Because PSVT is “paroxysmal” (occasional and sudden), an office ECG may look normal. To "catch" an episode, a doctor may suggest a portable heart monitor (Holter monitor or event monitor) to wear at home that will record your heart rhythm over time.
Treatment
Most people with SVT/PSVT don't need treatment. However, an episode may be stopped with one of these techniques, under the supervision of a health care professional. These affect the vagus nerve, which helps control the heartbeat.
- Carotid sinus massage: A health care professional applies gentle pressure on the neck where the carotid artery splits into two branches.
- Vagal maneuvers: Simple moves such as coughing or holding your nostrils closed while attempting to blow air through your nose.
- Dive reflex: This is the response by the body to plunging your face in ice-cold water. This is called a ‘Vagal maneuver’ It should only be done with a health care professional’s instruction.
Other treatments as needed:
- Medications: If you have frequent episodes of SVT, your health care professional may prescribe medication to control your heart rate or restore a typical heart rhythm.
- Cardioversion: This procedure delivers a shock to the heart, through patches or paddles to restore the normal heart rhythm.
- Catheter ablation: A doctor inserts thin, flexible tubes called catheters through the veins or arteries, usually in the groin. Sensors on the tip of the catheter use heat or cold energy to create tiny scars in the heart to block irregular electrical signals and restore a typical heartbeat.
Living With My Imperfect Heart

My Life With A Turbocharged Ticker

Sinus Tachycardia
Sinus tachycardia is an increase in the heart rate. In this condition, the heart’s natural pacemaker, the sinus node, sends out electrical signals faster than usual.
The heart rate is faster than normal, but the heart beats properly. It’s a common response to exercise, but it’s concerning when it occurs at rest.
Causes of sinus tachycardia
A rapid heartbeat may be your body’s response to common conditions such as:
- Anxiety
- Fright
- Severe emotional distress
- Strenuous exercise
- Fever
- Some medications and illegal drugs
- Pain
Other, less common causes may include:
- Anemia
- Infection
- Increased thyroid activity
- Heart muscle damage from heart attack or heart failure
- Severe bleeding
- Very low blood pressure
- Lung disease
Treatment
Your health care professional should consider and treat the cause of your sinus tachycardia, rather than just treating the condition. Simply slowing the heart rate could cause more harm if your rapid heartbeat is a symptom of a more serious or long-term problem.
Ventricular Tachycardia
Ventricular tachycardia (VT) is a fast heart rate that starts in the heart’s lower chambers (ventricles). Electrical signals in the heart’s lower chambers fire abnormally fast. This interferes with electrical impulses coming from the sinus node, the heart’s natural pacemaker.
The disruption results in a faster-than-normal heart rate. This rapid heartbeat keeps the heart’s chambers from filling completely between contractions, which reduce blood flow to the rest of the body.
VT may be either well-tolerated or life-threatening, requiring immediate diagnosis and treatment. The severity of VT depends largely on whether you have other heart conditions and the type of VT you have.
Causes of ventricular tachycardia
Ventricular tachycardia is most often associated with disorders that interfere with the heart’s electrical conduction system. These disorders can include:
- Lack of coronary artery blood flow, depriving oxygen to heart tissue
- Cardiomyopathy distorting the heart’s structure
- Medication side effects
- Use of illegal drugs such as cocaine or methamphetamine
- Sarcoidosis (an inflammatory disease affecting skin or body tissues)
- Abnormalities of the heart that result in scarring of heart tissue (sometimes called “structural heart disease”); the most common cause is a prior heart attack
- Congenital heart conditions, including long QT syndrome
- Imbalance of electrolytes needed for conducting electrical impulses
Symptoms
Symptoms for VT vary. Common symptoms include:
- Dizziness
- Palpitations
- Shortness of breath
- Nausea
- Lightheadedness
- Fainting (syncope)
- Cardiac arrest, in extreme cases
- Chest pain
Treatment
Treatment will depend on your symptoms and the cause of your VT. Possible treatments include:
- Medication that helps prevent arrhythmias
- Radiofrequency ablation, a procedure that destroys the cells causing the VT
- Surgery to implant a cardioverter defibrillator (ICD), which delivers an electrical pulse to the heart to reset a dangerously irregular heartbeat
- Immediate electrical defibrillation, in extreme cases
Additional resources: